Make an Appointment
Contact Us by Email
Spinal Cord Stimulation
Spinal cord stimulation uses low voltage stimulation of the spinal nerves to block the feeling of pain. It helps you to better manage your pain and potentially decrease the amount of pain medication. It may be an option if you have long-term (chronic) leg or arm pain, and have not found relief through traditional methods. A small battery-powered generator implanted in the body transmits an electrical current to your spinal cord. The result is a tingling sensation instead of pain. By interrupting pain signals, the procedure has shown success in returning some people to a more active lifestyle.
What is a spinal cord stimulator?
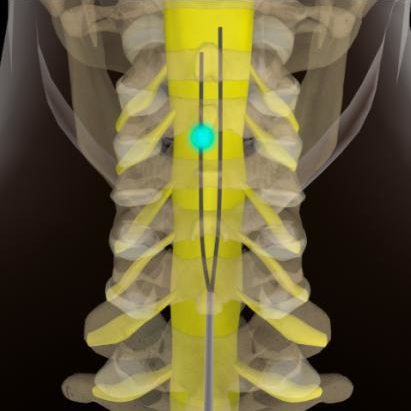
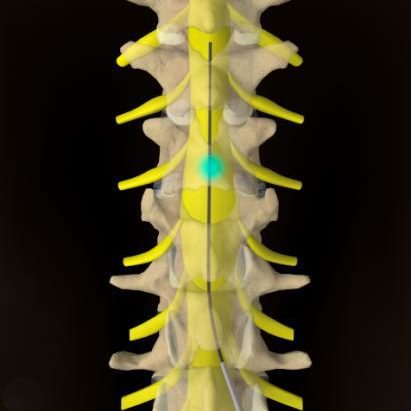
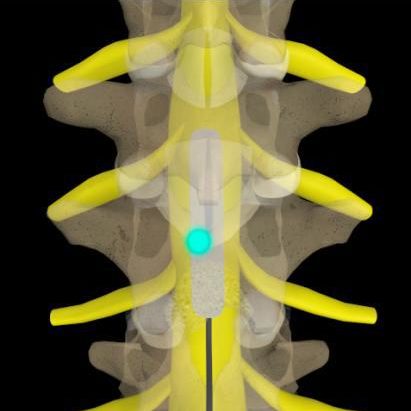
A spinal cord stimulator (SCS), also known as a dorsal column stimulator, is a device surgically placed under your skin to send a mild electric current to your spinal cord. A small wire carries the current from a pulse generator to the nerve fibers of the spinal cord. When turned on, the stimulation feels like a mild tingling in the area where pain is felt. Your pain is reduced because the electrical current interrupts the pain signal from reaching your brain.
Stimulation does not eliminate the source of pain, it simply interferes with the signal to the brain, and so the amount of pain relief varies for each person. Also, some patients find the tingling sensation unpleasant. For these reasons a trial stimulation is performed before the device is permanently implanted. The goal for spinal cord stimulation is a 50-70% reduction in pain. However, even a small amount of pain reduction can be significant if it helps you to perform your daily activities with less pain and reduces the amount of pain medication you take. Stimulation does not work for everyone. If unsuccessful, the implant can be removed and does not damage the spinal cord or nerves.
There are many types of stimulation systems. The most common is an internal pulse generator with a battery. A SCS system consists of:
- An implantable pulse generator with battery that creates electrical pulses.
- A lead with a number of electrodes (4-16) that delivers electrical pulses to the spinal cord.
- An extension wire that connects the pulse generator to the lead.
- A hand-held remote control that turns the pulse generator on and off and adjusts the pulses.
The battery inside the pulse generator delivers low voltage and needs to be surgically replaced every 2 to 5 years if it is a standard battery. Rechargeable battery systems may last up to 10 years, depending on usage. Your doctor will select the best type of system for you during the trial stimulation.
The pulse generator is programmable by the doctor and has three settings:
- Frequency (rate): number of times stimulation is delivered per second. Too few results in no sensation. Too many results in a washboard or bumpy effect.
- Pulse width: determines size of area stimulation will cover.
- Pulse amplitude: determines threshold of perception to pain.
Who is a candidate?
Before determining if spinal cord stimulation (SCS) is an option, your condition will be thoroughly evaluated and assessed. A comprehensive evaluation of your pain history will determine if your goals of pain management are appropriate to proceed with treatment.
Because pain also has psychological effects, a psychologist may assess your condition to increase the probability of a successful outcome. A neurosurgeon, pain specialist, or physiatrist will evaluate your current medication regime and physical condition. The doctor will want to review all previous treatments including medication, physical therapy, injections, and surgeries.
Patients selected for this procedure usually have had a disability for more than 12 months and have pain in their lower back and leg (sciatica). They’ve typically had one or more failed spinal surgeries.
You may be a candidate for SCS if you meet the following criteria:
- Conservative therapies have failed
- Your source of pain has been verified
- You would not benefit from additional surgery
- You are not seriously dependent on pain medication or other drugs
- You do not have depression or other psychiatric conditions that contribute to your pain
- You have no medical conditions that would keep you from undergoing implantation
- You have had a successful trial stimulation
An SCS can help lessen chronic pain caused by:
- Chronic leg (sciatica) or arm pain: ongoing, persistent pain caused by degenerative conditions like arthritis or spinal stenosis, or from nerve damage.
- Failed back surgery syndrome/ Post laminectomy syndrome: failure of one or more surgeries to control persistent leg pain (sciatica), but not technical failure of the original procedure.
- Complex regional pain syndrome (CRPS): a progressive disease of the nervous system in which patients feel constant chronic burning pain, typically in the foot or the hand. Formerly called reflex sympathetic dystrophy (RSD).
- Arachnoiditis: painful inflammation and scarring of the meninges (protective layers) of the spinal nerves.
- Other: stump pain, angina, peripheral vascular disease, multiple sclerosis, spinal cord injury.
If your pain is caused by a correctable condition, then this must be fixed first. Also, if you have a cardiac pacemaker, you cannot have a stimulator.
The surgical decision
Determining whether a spinal cord stimulator will be a good pain management option for you is a complex process. Before a permanent stimulator can be implanted, you must undergo a trial to see if the device decreases your level of pain.
The procedure is performed on an outpatient basis in two stages: Stage 1 is a trial stimulation and Stage 2 is implantation of the permanent device.
Stage 1. Trial stimulation
Trial stimulation is very important to determine if the procedure will be successful. It will tell if stimulation is correct for the type, location, and severity of your pain. It will also evaluate the effectiveness of various stimulation settings.
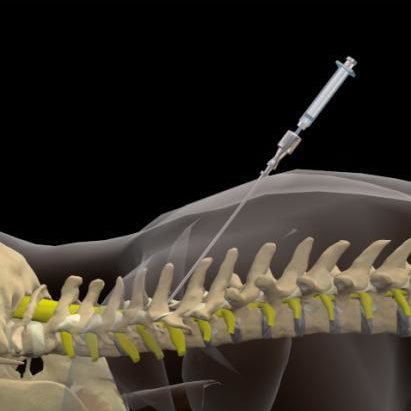
The insertion of a trial lead is typically performed under a local anesthetic. A hollow needle is inserted through the skin (percutaneous) into the epidural space between the bony vertebra and the spinal cord using fluoroscopy (a type of X-ray). The lead is properly positioned and then attached to an external generator and power supply (worn on a belt).
After the trial procedure, you will be sent home with instructions on how to use the trial stimulator and care for your incision site. Keep a written log of the stimulation settings during different activities and the level of pain relief. After 3 to 5 days, you will return to the doctor’s office to discuss permanently implanting the stimulator or removing the trial leads.
Stage 2. Permanent implantation
If the trial is successful and you experienced a greater than 50% improvement in pain, you can be scheduled for surgery. During the trial stimulation, your doctor gathered information about the number of electrodes needed and the type of stimulation that works best for you.
What are the results?
The results of spinal cord stimulation depend on strict patient selection, proper surgical technique, intra- and postoperative testing, and patient education. Stimulation does not cure the condition causing pain; it helps patients to tolerate pain.
Recent results of spinal cord stimulation show good to excellent long-term relief in 40 to 70% of patients suffering from chronic pain. One study reports that 24% of patients improved sufficiently to return to gainful employment or housework with stimulation alone or supplemented by occasional oral pain medication.
Living with a stimulator
Once the SCS has been programmed, you are sent home with instructions for regulating the stimulation by controlling the strength and the duration of each stimulation period. Your doctor may alter the pulse width, amplitude and frequencies on follow-up visits if necessary.
The handheld programmer lets you turn the stimulator on and off, select programs, and adjust the strength of the stimulation. Most people are given multiple programs to achieve the best possible pain relief during specific activities. You can use your spinal cord stimulator around the clock if necessary. However, most people get pain relief during the day and turn off the system before bedtime because pain relief often continues even after the stimulation has stopped. Everyone’s pain is different.
Some people feel differences in stimulation intensity depending on their position (e.g., sitting versus standing). This is caused by variations in the spread of electricity as you change positions and is normal. Do not use the stimulator while driving or swimming.
Just like a cardiac pacemaker, other devices such as cellular phones, pagers, microwaves, security doors, and anti theft sensors will not affect your stimulator. Be sure to carry your Implanted Device Identification card when flying, since the device is detected at airport security gates. Department store and airport security gates or theft detectors may cause an increase or decrease in stimulation when you pass through the gate. This sensation is temporary and should not harm your system. However, as a precaution, you should turn off your system before passing through security gates.
To avoid damage or adverse effects to your spinal cord stimulator, avoid the following medical procedures: MRI, ultrasound, defibrillator, electrocautery, diathermy, and cardiac pacemakers. Also, chiropractic manipulation may cause the lead to move – consult your surgeon first.