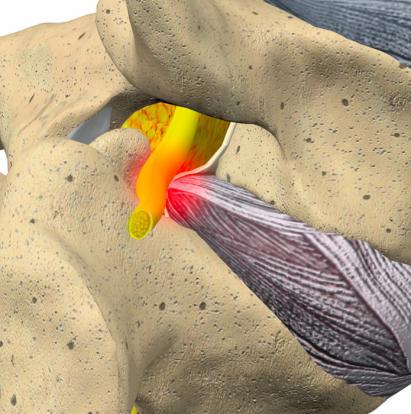
Sciatica or Radiculopathy is a condition that exists due to a compressed nerve in the spine that may cause numbness, pain, tingling or weakness along the path of the nerve.
Call 801-302-2690Contact UsThe body’s longest nerve, the Sciatic nerve is one of the most important. The Sciatic nerve has a direct correlation on your ability to control and feel your legs. If this nerve is irritated, you’ll experience sciatica.
Sciatica (Radiculopathy) is most common in the lower back (lumbar radiculopathy) and in the neck (cervical radiculopathy), although it can occur in any art of the spine. Patients who experience heavy labor on a normal basis are far more prone to radiculopathy than patients who live a more sedentary lifestyle. Most people obtain sufficient relief of their symptoms of radiculopathy with conservative treatment. Such treatment may include anti-inflammatory medications or physical therapy, and avoiding activity that puts a strain on the neck or back. The majority of radiculopathy patients have a positive response to this conservative treatment, and symptoms normally improve within the first six weeks. Typical treatments involve traditional conservative care to include anti-inflammatory medications, muscle relaxants, physical therapy, and avoiding activity that puts a strain on the neck or back. When pharmacologic and traditional non-pharmacologic therapies do not help, we at Wasatch Pain Solutions employ minimally invasive procedures that help reduce or eliminate this pain all together. In rare cases, surgery may be necessary, however we at Wasatch Pain Solutions feel that most cases do not require these costly invasive and medically complex surgical interventions. However, when appropriate you can be comforted in knowing that we will help navigate you to the best spine surgeons to treat your condition.
How does Prolotherapy work?
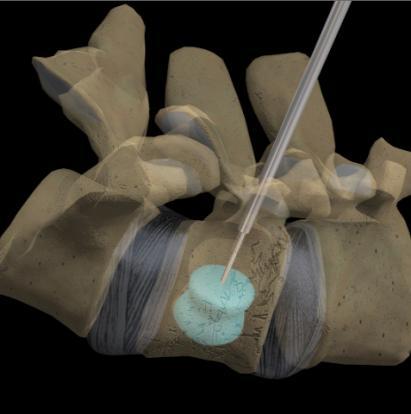
In vertebral compression fractures (VCF), the body collapses into itself (more in the front than the back) producing a “wedged” vertebra. When several vertebrae become wedge-shaped, people can develop a humped spine, called kyphosis. People with bones weakened by osteoporosis (a depletion of calcium) or multiple myeloma (cancer of the bone marrow) are especially prone to compression fractures. Activities, such as lifting a heavy object, sneezing, or coughing may cause fractures. VCFs can lead to back pain, reduced physical activity, depression, loss of independence, decreased lung capacity, and difficulty sleeping.
Vertebroplasty and kyphoplasty are similar procedures. Both are performed through a hollow needle that is passed through the skin of your back into the fractured vertebra. In vertebroplasty, bone cement (called polymethylmethacrylate) is injected through the hollow needle into the fractured bone. In kyphoplasty, a balloon is first inserted and inflated to expand the compressed vertebra to its normal height before filling the space with bone cement. The procedures are repeated for each affected vertebra. The cement-strengthened vertebra allows you to stand straight, reduces your pain, and prevents further fractures.
Without treatment, the fractures will eventually heal, but in a collapsed position. The benefit of kyphoplasty is that your vertebra is returned to normal position before the bone hardens. Patients who’ve had kyphoplasty report significantly less pain after treatment.
Studies show that people who get one osteoporotic fracture are 5 times more likely to develop additional fractures. It is important that people seek treatment for osteoporosis early, before fractures occur.
Is Kyphoplasty and Vertebroplasty right for you?

Vertebroplasty or kyphoplasty may be a treatment option if you have painful vertebral compression fractures from:
- Osteoporosis (a depletion of calcium in bones)
- Metastatic tumor (cancer spread from another area)
- Multiple myeloma (cancer of the bone marrow)
- Vertebral hemangioma (benign vascular tumor)
You may not be a candidate if you have:
- Non-painful stable compression fractures
- Bone infection (osteomyelitis)
- Bleeding disorders
- Allergy to medications used during the procedure
- Fracture fragment or tumor in the spinal canal
Vertebroplasty and kyphoplasty will not improve old and chronic fractures, nor will they reduce back pain associated with poor posture and stooping forward. Traditional treatment used to involve waiting 4 to 6 weeks to see if patients improved on their own, but now it’s believed that waiting allows the bone to harden, making vertebroplasty or kyphoplasty less effective. Many doctors are now suggesting vertebroplasty as soon as the first week after a fracture for some patients because the results are significantly better.
Thanks to Wasatch Pain Solutions, PA. Collin and Dr. Khan. I'm back on my Harley! I hadn't ridden in 2 years until after my hip injection! I highly recommend them! - Gary
Why Choose Wasatch?

DEDICATED CLINICAL STAFF

CUTTING-EDGE FACILITY

EXPERT SPINE EVALUATION

"" CLINIC